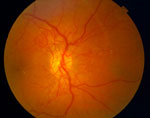
 People who have diabetes mellitus do not use and store blood sugar properly and the amount of sugar in the blood will be too high. High blood sugar levels can damage vessels in the retina. This damage is referred to as diabetic retinopathy.
People who have diabetes mellitus do not use and store blood sugar properly and the amount of sugar in the blood will be too high. High blood sugar levels can damage vessels in the retina. This damage is referred to as diabetic retinopathy.
There are two types of diabetic retinopathy:
NPDR (nonproliferative diabetic retinopathy), commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels (microaneurysms) within the retina leak blood or fluid. The leaking fluid causes the retina to swell or form deposits called exudates; white deposits within the retinal nerve fiber layer that represents small patches of the retina that have lost their blood supply, also called cotton-wool spots. Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected in NPDR it is the result of macular edema and/or macular ischemia.
Macular edema is swelling or thickening of the macular region, which usually results in a temporary reduction in visual acuity, though in some cases may be permanent. The macula is a small area in the retina which is responsible seeing fine details clearly. Macular ischemia occurs when small blood vessels close, causing vision to blur due to the macula no longer receiving a sufficient blood supply.
PDR (proliferative diabetic retinopathy), is an attempt by the eye to grow or re-supply the retina with new blood vessels (neovascularization), due to widespread closure of the retinal blood supply. Unfortunately, the new, abnormal blood vessels do not re-supply the retina with normal blood flow, but bleed easily and are often accompanied by scar tissue that may wrinkle or detach the retina. PDR can cause visual acuity loss in three ways:
Traction Retinal Detachment: Scar tissue associated with neovascularization can shrink surrounding tissue causing a wrinkle or tear, more severe visual acuity loss can occur if the macular region is affected.